Ocular Gene Therapeutics
As the in vivo gene therapy field has evolved, local injection in the anatomic site of interest has become an increasingly utilised approach with the intent of maximising exposure and chances of efficacy. while several organs systems have been investigated in nonclinical and clinical trials; the most notable attempts have been delivery to the eye.
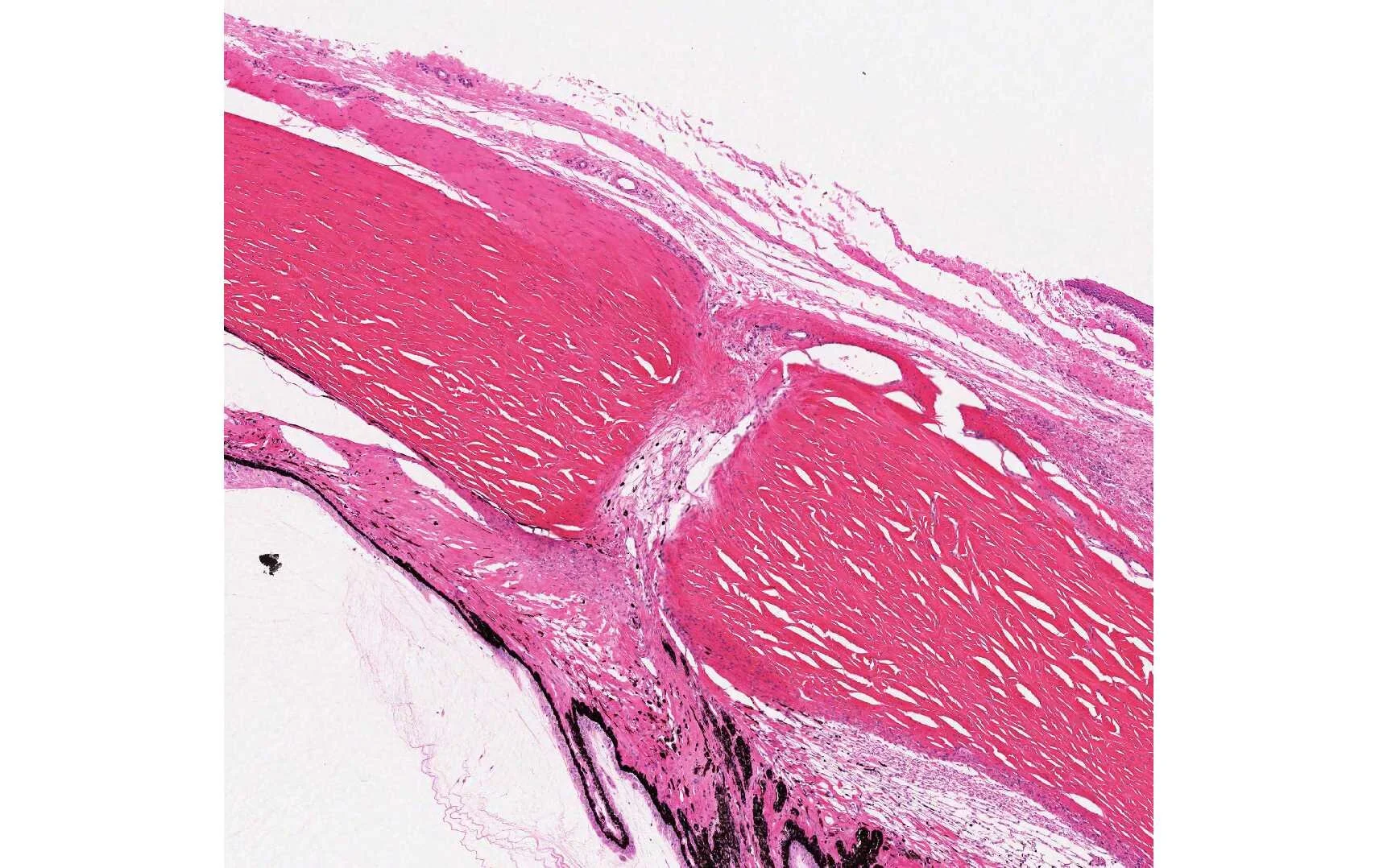
Needle Tract injections
Similarly, while Some investigators of ocular syndromes have Utilised the intra-vitreal route, more often, the gene therapy vector requires often a sub-retinal injection to reach photoreceptors and/or Retinal pigmented epithelia to treat Some of the genetic forms of blindness such as leber’s Congenital Amarousis (Boyle, 2013).
In any of these cases, it is important that the pathologist pay close attention to the Local health of the tissue near the injection site and should evaluate several timepoints after injection to differentiate between acute and chronic effect, if possible. Under certains circumstances, imaging modalities can Become very useful to the pathologist in reducing the number of animals in studies and the time and material required for standard histopathologically.
For example, technologies like ocular coherence tomography (OCT) (Baumal 1999) are able to generate near histopathology-grade images of retinal sublayers, allowing the pathologist to evaluate the effects of the injection and test article and recovery from such effects. Indeed, some retinal gene therapies have identified retinal thinning as an effect of the injection itself as well as the concentrate of the vector that was Administered (Jacobson 2006).
“Age-related Macular Degeneration is the leading cause of blindness in people over the age of 65. ”
the ‘wet’ form of AMD results in the most damage - often leading to blindness overnight from Haemorrhage under the retina Originating from blood vessels which have aberrantly entered this area (after traversing bruch’s membrane and the RPE. It has been difficult developing an animal models of wet ADM. this is because, as yet, no genes have been conclusively identified as causing this disease and also because the only animal with a macula is the primate. FlandersToxPath can help you with developing such animal models which can serve as Proof of Concept. The animal model implicates a mechanical rupture of bruch’s membrane with laser photocoagulation Which will stimulate CNV in primates, rabbits and rodents; however, lesions generated in this way generally resolve Spontaneously, unlike CNV found in humans with AMD.
Transgenic Rodents
Attempts have been made to generate transgenic rodents that Over express VEGF in photoreceptors. these animals develop neo-Vascularisation originating from the Virtual side of the retina, but no the choroid. Despite the imperfect animal models for the wet form of AMD, they have been useful in testing potential treatments for this disorder.
Gene therapy reagents have also been put to use to create an animal model so that medical treatments can be tested. recently, an Ad vector encoding human VEGF was used to induce CNV in the log-Evans rats. this viral vector was delivered sub-retinally and animals developed reproducible CNV 2 weeks post injection, suggesting it may be a useful model to study neo-vascularisation associated with AMD (Wissinger et al, 2003)
Ocular Gene Therapies
in december, 2017, the U.S. Food and Drug Administration approved a new gene therapy, voretigene neparvovec-rzyl (Luxturna) manufactured by Spark Therapeutics in Philadelphia. Luxturna is the first gene therapy approved in the United States that’s directly Administered into the eye, targeting diseases caused by mutations in the gene RPE65. Mutations in this gene can produce Leber’s congenital amourosos or retinitis pigmentosa, both Are potentially Blinding diseases.
Prof. Bennett, co-founder of Spark and scientific director for the RPE65 deficiecy trials said: ‘this is the second gene therapy Approved by the FDA, but it’s the first one to target a genetic disease, and the first in which the gene is delivered directly into the person, rather than first being delivered into a cell in a dish.It’s also the first gene therapy approved worldwide for a retinal disease.